Troubleshooting Tips for Ortho-K
Although there is a high first-fit success rate with Euclid MAX and Emerald designs, occasionally there is the need to improve the fitting relationship and to alter the topographical changes occurring. Here's a few tips to help the consultant determine what changes should be made for specific situations.
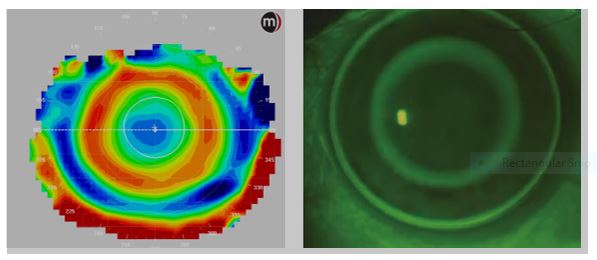
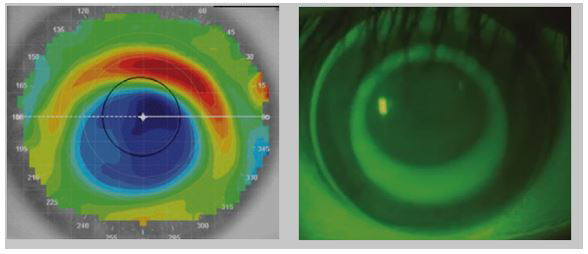
Ideal Fit
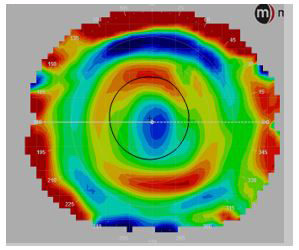
A properly fitted Euclid lens will show a well centered position on fluorescein and topography and provide the patient with their desired correction after 7-14 days of overnight wear.
Topographical Presentation: On topography, a well centered treatment pattern is seen as a complete red ring around the central cornea, commonly referred to as a "bullseye"
Fluorescein Presentation: The lens should move approximately 1-2mm with the blink, be centered over the cornea without impinging on the limbus, show a ring of fluorescein around the patient's pupil, and show sufficient edge lift 360 degrees.
Resolution: None required.
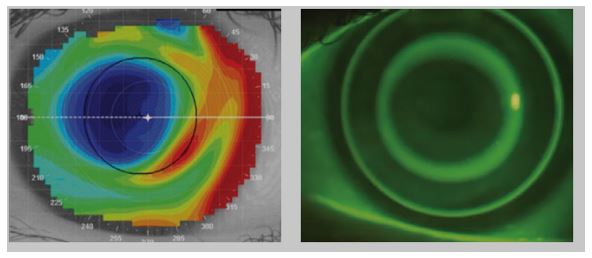
Superior Decentration
Superior decentration indicates that a lens has inadequate sagittal height and is too flat.
Topographical Presentation: On corneal topography, superior decentration is usually indicated by the appearance of a "smiley-face" pattern, where the treatment zone is higher than the pupil.
Fluorescein Presentation: The lens will usually be too tight and may move less than 1-2mm with the blink. You may see that the superior section of the lens is riding a few millimeters lower than the bottom of the patient's iris.
Resolution: If the patient does not have an astigmatic cornea (review Estimating Corneal Elevation Differences Using Corneal Astigmatism for more information), flatten the fit by flattening the alignment curves 0.1mm. If the patient is wearing a toric lens or has an astigmatic cornea, reduce toricity by 15 microns (~0.50D).
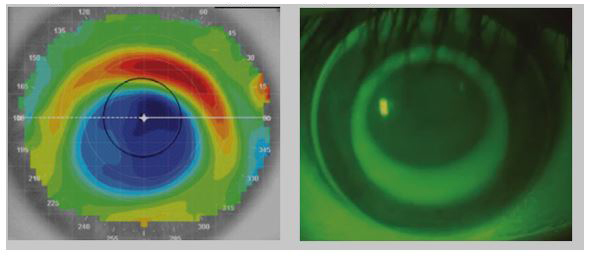
Inferior Decentration
Inferior decentration indicates that a lens has excessive sagittal height vertically and is too steep.
Topographical Presentation: On corneal topography, superior decentration is usually indicated by the appearance of a "frowny-face" pattern, where the treatment zone is lower than the pupil.
Fluorescein Presentation: The lens will usually be too tight and may move less than 1-2mm with the blink. You may see that the superior section of the lens is riding a few millimeters lower than the bottom of the patient's iris.
Resolution: If the patient does not have an astigmatic cornea (review Estimating Corneal Elevation Differences Using Corneal Astigmatism for more information), flatten the fit by flattening the alignment curves 0.1mm. If the patient is wearing a toric lens or has an astigmatic cornea, reduce toricity by 15 microns (~0.50D).
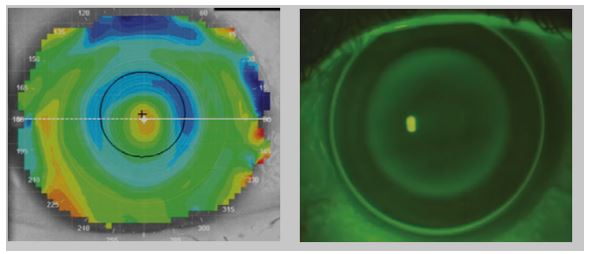
Lateral Decentration
Lateral decentration usually indicates the lens diameter is too small.
Topographical Presentation: On corneal topography, lateral decentration is usually indicated by the appearance of a crescent shape that intersects with the central cornea.
Fluorescein Presentation: The lens may be positioned laterally, with one peripheral edge of the lens resting in the interior cornea and one edge resting on or near the sclera.
Resolution: If the patient's HVID can tolerate a larger lens (see Determining Overall Lens Diameter (OAD) for more information), increase the overall diameter (OAD) by one step (0.4mm). If the patient's HVID cannot tolerate a larger lens, consider the use of a 0.75D toric lens design instead.
Central Islands
Central islands usually indicate the lens has excessive sagittal height.
Topographical Presentation: On corneal topography, central islands are usually indicated by the appearance of a steep central area resembling an island.
Fluorescein Presentation: The lens may show central pooling underneath the reverse curve, with no clear bullseye.
Resolution: Flatten the reverse curve by one step (0.2mm) to resolve.
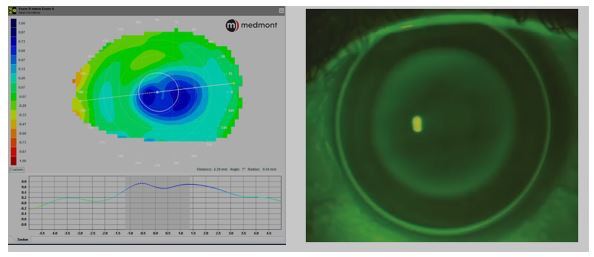
Central Vaulting
Vaulting usually indicates the lens has excessive sagittal height.
Topographical Presentation: On corneal topography, vaulting is usually indicated by the appearance of a central treatment zone without 360 degrees of even flattening. The treatment zone may appear oval or have a pattern of bowtie astigmatism. For the best diagnosis, use an axial difference map to evaluate the treatment zone. Using a post-treatment map only may result in a misdiagnosis of lens vaulting.
Fluorescein Presentation: The lens may show central pooling underneath the reverse curve, with no clear bullseye.
Resolution: Flatten the reverse curve by one step (0.2mm) to resolve.
Insufficient Treatment
In some cases, patients may experience insufficient treatment or correction of their myopia unrelated to lens decentration or excessive/insufficient sagittal height.
Topographical Presentation: On corneal topography, insufficient treatment usually presents as an Ideal Fit.
Fluorescein Presentation: Insufficient treatment usually presents as an Ideal Fit.
Resolution: Increase the target correction (flatten the base curve) by the amount of the under-correction. For example, if a patient with an original Rx of -3.00D is getting a residual Rx of -0.50D after 14 days of lens wear, increase the target correction 0.50D for a new target of -3.50D.
Glare, Haloes and Ghosting
Glare, haloes, and ghosting are a common side effect of ortho-k lens wear. These side effects typically present in dim light conditions due to the expansion of the pupil outside of the effective treatment zone of the ortho-k lenses.
Glare and haloes are typically present at the beginning of ortho-k wear as a patient’s corneas adjusts to the reshaping effect and may resolve with continued lens wear. If glare and haloes persist after a month of lens wear, consider changing the lens to improve this condition.

Glare and haloes are not typically reported by younger patients (ages 6-15), as they do not usually have demanding night vision needs. Older patients (ages 16+) may notice issues with glare and haloes when they begin driving or spending a great deal of time in low light conditions. While some research indicates that smaller optic zones may provide better myopia management (see Clinical Guidance: Posterior Optic Zone Diameters for more details), the risk of myopic progression typically slows after the age of 16.
Topographical Presentation: Topographies may show a very small treatment zone with a reverse curve that is partially or fully encapsulated within the patient's pupil.
Fluorescein Presentation: No specific presentation.
Resolution: If myopia management is not the primary goal of treatment and the lenses are not decentered, consider increasing the posterior optic zone size 0.4mm. The largest optic zone size available in Euclid's ortho-k lens designs is 6.6mm. If myopia management is the primary goal of treatment, discuss the potential trade-offs of choosing a larger treatment zone vs. a smaller treatment zone. If the lens is decentered, follow instructions for resolving decentration before changing the optic zone size.
Lens Warpage
Euclid's orthokeratology lenses expire one year after the date of manufacture. This expiration date is based on internal shelf-life testing. As a result, Euclid recommends patients replace their lenses yearly. Please see the Clinical Guidance for Routine OrthoK Lens Replacements for more details on the mechanical damage lenses can experience over time.
Lenses that have been worn for more than a year can become warped or damaged over time, resulting in a lens that doesn't provide adequate vision or comfort for the patient. In a consult, this can manifest as residual spherical error, induced astigmatism, lens decentration, or patient discomfort. Lens warpage can occur in all parameters of the lens, including the base curve and alignment curves.
If you are performing a consult on a pair of lenses that are substantially more than a year old (two+ years), it can be beneficial to recommend a fresh pair of lenses before making any changes. If the lenses are not substantially more than a year old, it's important to work with the customer to determine the best change required for the lenses. While a fresh pair may solve the problem, there may be an underlying problem with the lens fit as well. Sometimes it can be helpful to split the difference with any changes so that you are making a smaller change. For example, if the patient is experiencing uncorrected spherical error of -1.00D, you might suggest flattening the base curve (increasing the target) -0.50D instead of -1.00D.
Remember that our customers' chair time is very valuable, so it's important to work with them to minimize return visits. If you recommend replacing the lenses with no changes and they would like to make a change, make sure to recommend changes accordingly.